If you are seeing the 3 F's, you might have a retinal tear or detachment and you should have an eye exam quickly.
The 3 F's are:
- Flashes - flashing lights.
- Floaters - dozens of dark spots that persist in the center of your vision.
- Field cut – a curtain or shadow that usually starts in peripheral vision that may move to involve the center of vision.
The retina is the nerve tissue that lines the inside back wall of the eye and if there is a break in the retina, fluid can track underneath the retina and separate it from the eye wall. Depending on the location and degree of retinal detachment, there can be very serious vision loss.
If you have a new onset of any of the three symptoms above, you need to get in for an appointment fairly quickly (very quickly if there are two or more symptoms).
If you have just new flashes or new floaters you should be seen in the next few days. If you have both new flashes and new floaters or any field cut, you should be seen in the next 24 hours.
When you go to the office for an exam, your eyes will be dilated. A dilated eye exam is needed to examine the retina and the periphery. This may entail a scleral depression exam where gentle pressure is applied to the outside of the eye to examine the peripheral retina. Some people have a hard time driving after dilation--since the dilating drops may last up to 6 hours, you may want to have someone drive you to and from your appointment.
If the exam shows a retina tear, treatment would be a laser procedure to encircle the tear.
If a retinal tear is not treated in a timely manner, then it will progress into a retinal detachment. There are four treatment options for retinal detachment:
- Laser. A small retinal detachment can be walled off with a barrier laser to prevent further spread of the fluid and the retinal detachment.
- Pneumatic retinopexy. This is an office-based procedure that requires injecting a gas bubble inside the eye. The patient then needs to position his or her head for the gas bubble to reposition the retina back along the inside wall of the eye. A freezing or laser procedure is then performed around the retinal break. This procedure has about 70% to 80% success rate, but not everyone is a good candidate for a pneumatic retinopexy.
- Scleral buckle. This is a surgery that needs to be performed in the operating room. This procedure involves placing a silicone band around the outside of the eye to bring the eye wall closer to the retina. The retinal tear is then treated with a freezing procedure.
- Vitrectomy. In this surgery, the gel - the vitreous inside the eye - is removed and the fluid underneath the retina is drained. The retinal tear is then treated with either a laser or freezing procedure. At the completion of the surgery, a gas bubble fills the eye to hold the retina in place. The gas bubble will slowly dissipate over several weeks. Sometimes a scleral buckle is combined with a vitrectomy surgery.
Prognosis
The final vision after retinal detachment repair is usually dependent on whether the center of the retina - called the macula - is involved. If the macula is detached, then there is usually some decrease in final vision after reattachment. Therefore, a good predictor is initial presenting vision. We recommend that anyone with symptoms of retinal detachments (flashes, floaters, or field cuts) have a dilated eye exam. The sooner the diagnosis is made, the better the treatment outcome.
Article contributed by Dr. Jane Pan
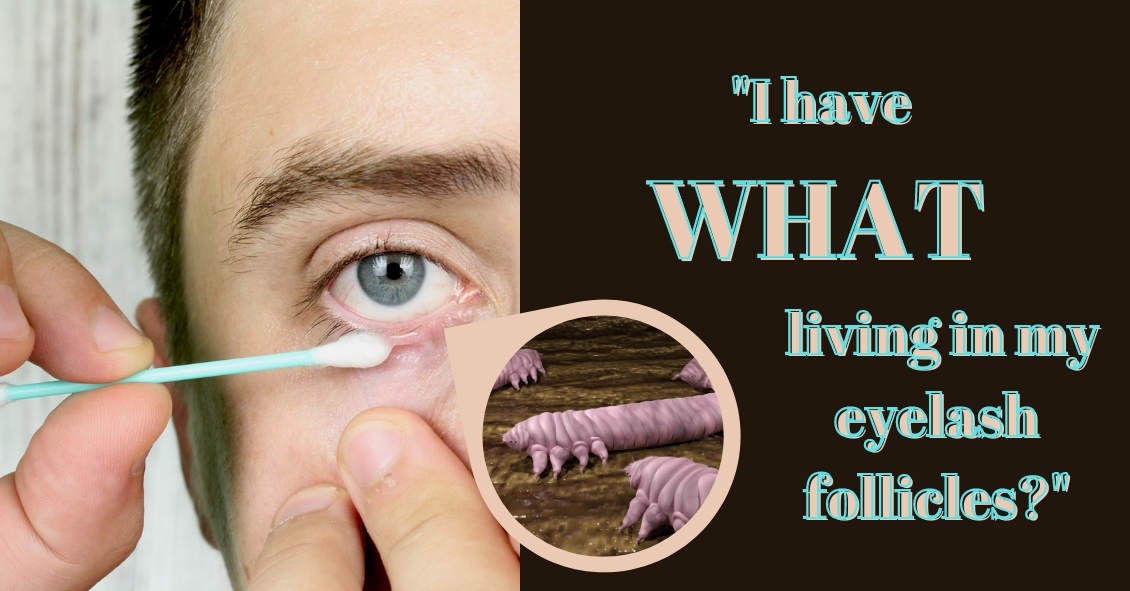 Demodex folliculorum -- often just called demodex -- is a mite that occurs naturally on many people's faces and resides in hair follicles, particular...
Demodex folliculorum -- often just called demodex -- is a mite that occurs naturally on many people's faces and resides in hair follicles, particular...


